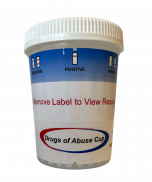
iCup One Step Drug Test Cups - 13 Panel
(25 Cups)
Now in Stock!
iCup One-Step Drug Test Cup- 13 Panel. One-step fully integrated iCup for detection of 13 major drugs of abuse in urine. This test cup will detect marijuana, cocaine, opiates, methamphetamines, amphetamines, PCP, barbiturates, benzodiazepines, propoxyphene, MTD, oxycodone, TCA and buprenorphine.
Ground Shipping Only!
For expediated shipping please email [email protected] or call 888.882.7739 to place your order.
NOTE: ALL ORDERS SHIPPING OUTSIDE 48 CONTINENTAL USA STATES INCLUDING APO’S WILL INCUR ADDITIONAL S&H FEES. A CUSTOMER SERVICE REPRESENTATIVE WILL CONTACT YOU FOR ANY INCREASED FREIGHT EXPENSES.
FDA-cleared and CLIA-classified as moderately complex (NOT CLIA-waived). (FDA#K061718)
CALL 888-882-7739 FOR VOLUME PRICING! No refunds or exchanges.
Detects the presence of drugs. It's drug testing efficiency you can count on.
Integrated testing solution:
- iCup® with temperature strip
- Two-part result form available
- Security Seal
- Photocopy Template
Benefits:
- Room temperature storage
- Built-in validity test
- Detects 5 drugs
- Simple procedure
- Fast results
- 12-18 Month Shelf Life
- FDA Cleared / CLIA waived, NOTE: 13-panel cup is Moderate Complex
|
Drug Name: |
Abbr: |
Cutoff: |
|
Amphetamine |
AMP |
1000ng/mL |
|
Barbiturates |
BAR |
300ng/mL |
|
Benzodiazepines |
BZO |
300ng/mL |
|
Cocaine |
COC |
300ng/mL |
|
Ecstasy |
MDMA |
500ng/mL |
|
Marijuana |
THC |
50ng/mL |
|
Methadone |
MTD |
300ng/mL |
|
Methamphetamine |
mAMP |
1000ng/mL |
|
Morphine |
MOR |
300ng/mL |
|
Opiates |
OPI |
2000ng/mL |
|
Oxycodone |
OXY |
100ng/mL |
|
Phencyclidine |
PCP |
25ng/mL |
|
Propoxyphene |
PPX |
300ng/mL |
|
Tricyclic Antidepressants |
TCA |
1000ng/mL |
CPT Code*: 80305 - Drug test(s), presumptive, any number of drug classes, qualitative; any number of devices or procedures, (e.g., immunoassay) capable of being read by direct optical observation only (e.g., dipstick, cups, cards, cartridges) includes sample validation when performed, per date of service (maps to 80300 or G0477).
National Average Reimbursement 2019: $12.60
*All CPT codes are supplied for information purposes only and represent no statement; promise or guarantee by CLIAwaivedTM Inc. that these codes will be appropriate or that reimbursement will be made. It is the responsibility of the service provider to confirm the appropriate coding required by their local Medicare carriers, fiscal intermediaries and commercial payors.